Billing
Phone: 888.444.0476
Email: UTPbilling@utoledo.edu
Patient Estimates
Mail Payment
UNIVERSITY OF TOLEDO PHYSICIANS
PO Box L-4189
Columbus, OH 43260-4189
(Checks Payable to: UNIVERSITY OF TOLEDO PHYSICIANS, LLC)
Online Payment
Is My Bill From the University of Toledo Physicians or UTMC?
The University of Toledo Medical Center and the University of Toledo Physicians function off of Provider Based Billing (PBB). PBB is a national model of billing practice that is regulated by CMS (Centers for Medicare & Medicaid Services). PBB refers to the billing process for services that are rendered in an outpatient clinic (department) of the hospital. In simple terms, the professional services and the facility overhead expenses are billed separately.
How does provider-based billing (PBB) affect copayments, coinsurance, and deductibles?

Why is the same procedure/service code (CPT code) used twice?
For services rendered in a PBB clinic (or in any hospital outpatient department for that matter), the reason that you see the same CPT code on both the hospital bill and on the physician’s bill is this:
- The code on the hospital bill represents all of the overhead expense incurred to perform that service/procedure and is submitted as a “facility” claim. Examples of overhead expenses are the rent on the building, the cost of the exam table, the disposable supplies, the salaries of the support staff, etc.
- The same code on the healthcare provider’s bill represents the physician or non-physician practitioner’s personally-performed, professional work to perform that procedure and is submitted as a “professional” claim.
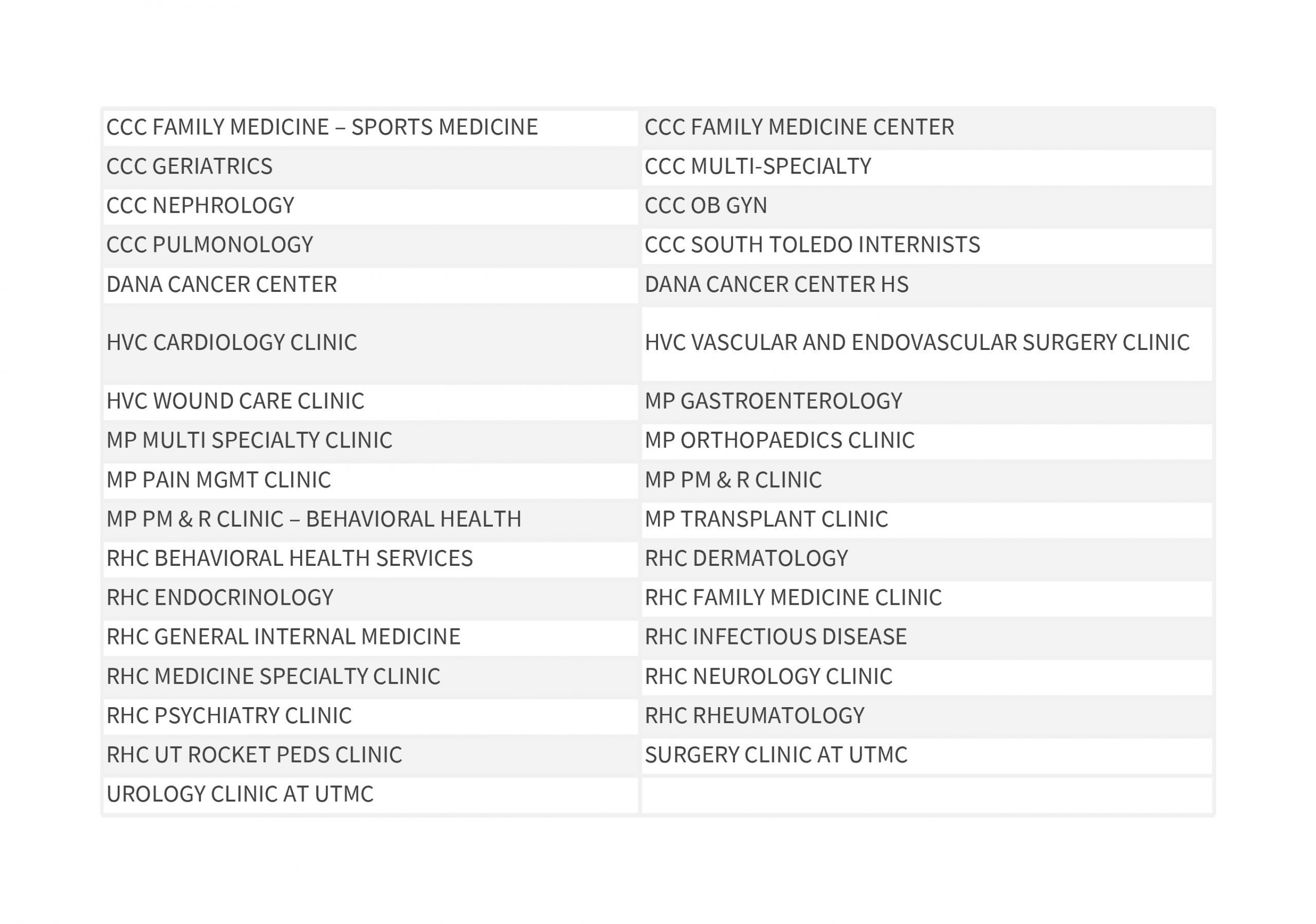
CCC= Comprehensive Care Clinic
MP= Medical Pavilion
RHC= Ruppert Health Center
HVC= Heart and Vascular Center
Payers Affected By PBB
- Traditional Medicare (Includes RR Medicare)
- State Medicaid
- Medicaid Managed Care Plans
- Workers Comp
- AETNA -All Products
- Self Pay Patients
Billing Terms
Advanced Beneficiary Notice (ABN)
A form to be signed for any services not covered by Medicare, making the patient financially responsible.
Billing Statement
Summary of patient account activity that is sent to patient or parents/guardians updating them regarding the status of their claim.
Claim
The information billed to the insurance company for services provided to you.
Contractual
The difference between the insurance contracted amount and the amount of the charge.
Copayment or Coinsurance
The fee per visit paid by the patient for healthcare services as determined by your medical insurance policy.
Deductible
The amount that the patient must pay for healthcare services before the insurance policy begins making payments. The health insurance policy sets this amount; usually it is due every calendar year.
EOB (Explanation of Benefits)
A detailed explanation of coverage from the insurance company for the medical services provided to you.
Financial Assistance
Adjustments made for qualified responsible parties, based on financial assistance applications and established financial guidelines.
Guarantor
The person – self, parent/guardian – responsible for payment of services provided not covered by insurance(s).
Managed Care
A medical delivery system that manages the quality and cost of medical services.
Medicaid
The joint federal / state program that provides healthcare insurance to low-income families.
Medicare Secondary Payer (MSP)
A federally mandated series of questions that Medicare patients will be asked prior to each visit.
Payment Arrangements
A formal payment plan set up with a Financial Counselor or Patient Financial Services when the balance due cannot be entirely paid by the due date.
Payer
A third party entity (commercial or government) that pays medical claims.
Prior Authorization / Pre-certification
A formal approval obtained from the insurance company prior to delivery of medical services. Many insurance companies require prior authorization or pre-certification for specific medical services.
Subscriber
The person who holds and / or is responsible for the medical insurance policy.
My Insurance Coverage
Thank you for choosing The University of Toledo Physicians. We are committed to clinical excellence and innovation in meeting your healthcare needs. We understand that billing and payment for healthcare services can be confusing and complicated. We are here to assist you with information on how we process your bill(s). The information below is designed to help you understand what we can do to assist you, what you can do to assist us and your insurance plan, and how we can help if you have difficulty in paying your bills.
When You Come to the Hospital or Clinic
The University of Toledo Physicians participates with most insurance companies, including Medicare and Medicaid. Prior to your hospital or clinic visit, check with your employer or insurance company to see if you have access to healthcare services provided by The University of Toledo Physicians, otherwise you may be responsible for all or a large portion of your bill.
Please Understand and Follow the Requirements of Your Health Plan
Be sure to know your benefits, obtain proper authorization for services, submit referral or claim forms, or fill out a coordination of benefits form, if necessary. Copayment and the deductible amount may be due at the time of registration or at the time of service. Please come to your appointment prepared to make a copayment or payment toward the outstanding balance due. You are responsible for paying copayments required by your insurance provider, and The University of Toledo Physicians is responsible for collecting copayments.
Out of Network
In an emergency, always go to the closest hospital. Your insurance provider generally will cover emergency department costs or transfer you to an “in-network” hospital if it is safe to do so. If you choose to go to an “out-of-network” hospital in a non-emergency, you may be required to pay a larger deductible or a greater portion of your bill. Be sure you understand your health plan’s “out-of-network” options.
Inform Us of Changes
If you are a current patient, please inform us if your personal or insurance information has changed since your last visit. The lack of current information can cause payment delays or denials that may ultimately leave you responsible for payment.
Making Deposits
For certain procedures not covered by insurance, you may be required to pay a deposit or pay for the service in full prior to your care.
Consent = Financial Responsibility
The person who consents to medical treatment will be financially responsible for the bill, including legal guardians of a child.
Medicare Patients: What to Expect
If you are a Medicare patient, you will be asked a series of questions regarding your status including other insurance you may have and your retirement. These Medicare Secondary Payer (MSP) questions are required by law and must be asked each time you visit us. If you are covered by Medicare, we will submit your claims to Medicare on your behalf.
When Medicare Doesn’t Cover a Service
Medicare requires we provide only those services approved by Medicare as deemed medically necessary. In the event the service is not covered by Medicare, we may ask you to sign an Advance Beneficiary Notice (ABN) that may make you financially responsible for the services provided. Additionally, we will bill you and/or your supplemental insurance carrier for services not covered by Medicare such as self-administered medications and routine health exams. However, if neither covers these services you will be responsible for payment for these services.
Financial Assistance or Payment Plans
If you anticipate problems paying your portion of your bill, please let us know. We can help you apply for other types of financial assistance or payment plans.
After Your Visit
Respond promptly to requests from your insurance company for additional information. These requests must be handled before payment can occur.
Call Us With Billing Questions
If you have any questions about your bill(s), please contact Financial Services Monday through Friday from 8:00 a.m. until 4:30 p.m. Please call 888.444.0476 You may also email UTPbilling@utoledo.edu with questions.
Who Can Discuss a Bill
Confidentiality is important. Our representatives may only speak with the patient or the person designated in writing by the patient to receive the bill(s) on behalf of the patient. This is required by both federal and state law.
Bring Your Health Insurance Information
Bring your complete health insurance information when you register. This includes identification, all insurance cards, and authorization forms. We will ask you to sign forms, such as a release of information, and possible additional forms depending on your visit.
Making Co-Payments
Copayments for both physician and hospital care and other balances you may owe are due on the day you receive services. If your insurance requires it, you will need to pay for estimated coinsurance or deductibles related to your care. If you have any questions regarding your copayments or deductibles, please call your insurance company.
Annual Wellness Visits (AWVs), Initial Preventive Physical Examinations (IPPEs) and Routine Examinations
Medicare may cover two specialized physical examination services for eligible beneficiaries: the Initial Preventive Physical Examination (IPPE) and an Annual Wellness Visit (AWV). When eligible for Medicare reimbursement, these services are covered at no cost to beneficiaries; coinsurance and deductible do not apply. There are specific required elements and coverage criteria for both IPPEs and AWVs. Please contact your provider’s clinic or our Patient Access Center if you want to schedule an IPPE or AWV.
In general, Medicare does not pay for “routine examinations.” These services are designated as status N in the Medicare Physician Fee Schedule Database (MPFSDB) and are never reimbursed by Medicare. It is important to note that these CPT codes are not appropriate codes for submitting AWV or IPPE services.
Can’t Pay Your Bill?
If you have any questions regarding your services, please call 888.444.0476 for assistance.
You may also email UTPbilling@utoledo.edu with any questions.
Frequent Questions Regarding Bills and Statements
If you need additional information, please contact Patient Financial Services at UTP:
Phone: 888.444.0476
Email: UTPbilling@utoledo.edu
Fax: 419.383.2000
Q. I received a billing statement. How do I know my insurance company paid its portion?
A. If you have any questions about your insurance payment, please call your insurance company directly. The insurance company’s phone number is usually printed on the back of your insurance card.
Q. When do I pay the copayment?
A. Your copayment is due when you register. If you are unsure of your co-pay responsibilities, please look at your insurance card, or call your insurance company.
Q. How does my insurance company receive the claim for healthcare services?
A. The University of Toledo Physicians files the claim with your insurance company. To ensure prompt, proper claim processing, please verify The University of Toledo Physicians has the proper insurance information on file when you register.
Q. Why do I receive two (2) billing statements when I only see a physician at The University of Toledo Physicians?
A. With most physician-related services performed at The University of Toledo Medical Center by UTP Physicians, there is a corresponding hospital facility fee. This is because the services are performed at the hospital (or a hospital outpatient center) and not in an independent physician’s office.
Q. Why are some of my bills covered by my insurance, while others are not covered?
A. Coverage can change every year depending on your benefit plan. This determines whether or not a patient’s bill is covered by insurance. Health coverage often has a deductible or out-of-pocket expense. Since each plan can be different, we encourage patients to carefully review their benefits with their insurance company.
Q. Why do I receive billing statements from the hospital when I was never there?
A. The University of Toledo Physicians provides a wide array of medical-related services for independent clinics and physicians, as well as other hospitals.
For example, a physician or a free-standing health center may refer lab work to The University of Toledo Physicians for testing or analysis. When this occurs, the bill for the lab services will come from The University of Toledo Physicians and not the physician or health center.
Q. My medical bills are adding up fast, and I can’t afford to pay them. How can I get help?
A. We are committed to providing healthcare to individuals, regardless of family income.
Please call Patient Financial Services at 888.444.0476 to discuss financial assistance options. You may also email UTPbilling@utoledo.edu with any questions. Our Patient Financial Services Representatives can help you apply for financial assistance.
If you are experiencing financial hardship, please complete our financial hardship form and email to UTPbilling@utoledo.edu.
Download Financial Hardship Application
Q. I received a letter stating my account has been referred to a collection agency or collection attorney. Why was this done and what should I do?
A. Before an account is placed with a collection agency, you will receive billing statements from The University of Toledo Physicians advising you of your account activity. You may also receive phone calls from The University of Toledo Physicians during this billing period. Once an account is placed with an outside collection agency, we ask that you work directly with the agency to resolve the balance.
Q. Do you bill my secondary insurance?
A. Patient Financial Services does bill your secondary insurance company provided it was provided at the time of your service. Please give your secondary insurance a chance to pay after your primary insurance has paid before you call Patient Financial Services. Generally, the secondary insurance will pay within 4 weeks after your primary insurance pays.
Q. What’s the difference between Medicare and Medicaid?
A. Medicare is a federal program you pay into and can collect at age 65. You will receive a monthly statement after Medicare processes your claim and notifies you of the amount you owe. Medicaid is a state program based on your income and needs. You will only receive a statement if we do not have your current Medicaid billing information. If you are covered by Medicaid and receive a statement, please call Patient Financial Services immediately at 888.444.0476. You may also email UTPbilling@utoledo.edu with questions.
Q. Why does it take so long to get a statement showing what I owe?
A. Generally statements are not generated until all of your insurance companies have responded or made payments. If you have not received an explanation of benefits from your insurance company within 35 days of your visit, please contact them for the status on your claim.
Q. Who is responsible for payment?
A. The patient or legal guardian is ultimately responsible for costs incurred for care. Once your information is received, The University of Toledo Physicians will make every effort to collect from your insurance companies or government agencies. It is your responsibility to contact your insurance companies to ensure prompt payment.
Q. Does my bill cover all the charges incurred for my treatment?
A. Not necessarily. The bill you receive from The University of Toledo Physicians covers only the cost of physician services and/or interpretation of tests and X-rays. It is important that you ensure that each of these physicians participates in your insurance plan. To find out if they participate, please contact the office of the billing physician. The results of all tests and / or X-rays will be forwarded to the ordering physician.
Q. If my statement says that the bill was rejected by my insurance what should I do?
A. Contact your insurance company first to find out why they rejected it. If The University of Toledo Physicians needs to resubmit the bill or send more information, please call Patient Financial Services at 888.444.0476. You may also email UTPbilling@utoledo.edu with questions.
Q. How can I be sure my insurance provider will pay my bills?
A. Some health plans require certain services to be authorized, or pre-certified, before the patient receives them. Other health plans require the patient to notify them within a certain period of time after services are rendered. Know your health plan’s requirements by reading the information given to you by your insurance provider or employer, or by calling your insurance provider directly.
Q. I’m an uninsured patient. What am I required to do?
A. Uninsured patients may be required to deposit the estimated cost of scheduled services in advance. If additional testing, physician consultations or hospital admissions are necessary, additional deposits may be required. If you are experiencing financial hardship, please complete our financial hardship form and email it to UTPbilling@utoledo.edu.
Q. What if my insurance company has no contractual agreement with The University of Toledo Physicians?
A. If you are a customer of a private insurance company that does not have a contractual agreement with The University of Toledo Physicians, you can still receive treatment. However, you will be financially responsible for the total charges and may be asked to make a deposit prior to receiving treatment. It is your responsibility to know what your insurance will cover and will not cover. To see if The University of Toledo Physicians is contracted with your insurance company, please call Patient Financial Services at 888.444.0476 to discuss financial assistance options.
Learn More About Insurance Eligibility
If there are any questions regarding your insurance, please contact our team. Please call 888.444.0476. You may also email UTPbilling@utoledo.edu with questions.
Your Rights and Protections Against Surprise Medical Bills
When you get emergency care or are treated by an out-of-network provider at an in-network hospital or ambulatory surgical center, you are protected from balance billing. In these cases, you shouldn’t be charged more than your plan’s copayments, coinsurance and/or deductible.
What is “balance billing” (sometimes called “surprise billing”)?
When you see a doctor or other health care provider, you may owe certain out-of-pocket costs, like a copayment, coinsurance, or deductible. You may have additional costs or have to pay the entire bill if you see a provider or visit a health care facility that isn’t in your health plan’s network.
“Out-of-network” means providers and facilities that haven’t signed a contract with your health plan to provide services. Out-of-network providers may be allowed to bill you for the difference between what your plan pays and the full amount charged for a service. This is called “balance billing.” This amount is likely more than in-network costs for the same service and might not count toward your plan’s deductible or annual out-of-pocket limit.
“Surprise billing” is an unexpected balance bill. This can happen when you can’t control who is involved in your care—like when you have an emergency or when you schedule a visit at an in- network facility but are unexpectedly treated by an out-of-network provider. Surprise medical bills could cost thousands of dollars depending on the procedure or service.
You’re protected from balance billing for:
Emergency services
If you have an emergency medical condition and get emergency services from an out-of- network provider or facility, the most they can bill you is your plan’s in-network cost-sharing amount (such as copayments, coinsurance, and deductibles). You can’t be balance billed for these emergency services. This includes services you may get after you’re in stable condition, unless you give written consent and give up your protections not to be balanced billed for these post-stabilization services.
Ohio law protects patients covered by state-regulated insurance plans and insurance plans subject to the jurisdiction of the superintendent of insurance from balance-billing for covered emergency services provided by an out-of-network provider at an out-of-network emergency facility and at an in-network emergency facility. These protections require patients to pay only their in-network cost-sharing amounts. For more information, see Ohio Rev. Code §§ 3922.01, 3902.50, 3902.51.
Certain services at an in-network hospital or ambulatory surgical center
When you get services from an in-network hospital or ambulatory surgical center, certain providers there may be out-of-network. In these cases, the most those providers can bill you is your plan’s in-network cost-sharing amount. This applies to emergency medicine, anesthesia, pathology, radiology, laboratory, neonatology, assistant surgeon, hospitalist, or intensivist services. These providers can’t balance bill you and may not ask you to give up your protections not to be balance billed.
If you get other types of services at these in-network facilities, out-of-network providers can’t
balance bill you, unless you give written consent and give up your protections.
You’re never required to give up your protections from balance billing. You also aren’t required to get out-of-network care. You can choose a provider or facility in your plan’s network.
Ohio law protects patients covered by state-regulated insurance plans and insurance plans subject to the jurisdiction of the superintendent of insurance from balance-billing for covered services provided by an out-of-network provider at an in-network facility if a patient did not have the ability to request an in-network provider. These protections require patients to pay only their in-network cost-sharing amounts. For all other medical services provided to a covered patient by an out-of-network provider at an in-network facility, a patient cannot be balance-billed unless the patient is informed, provided with a good faith estimate of the cost of the healthcare services, and consents. For more information, see Ohio Rev. Code §§ 3922.01, 3902.50, 3902.51.
If you believe you’ve been wrongly billed, you may contact the Ohio Department of Insurance at 800- 686-1526.
When balance billing isn’t allowed, you also have these protections:
• You’re only responsible for paying your share of the cost (like the copayments, coinsurance, and deductible that you would pay if the provider or facility was in-network). Your health plan will pay any additional costs to out-of-network providers and facilities directly.
• Generally, your health plan must:
o Cover emergency services without requiring you to get approval for services in advance (also known as “prior authorization”).
o Cover emergency services by out-of-network providers.
o Base what you owe the provider or facility (cost-sharing) on what it would pay an in-network provider or facility and show that amount in your explanation of benefits.
o Count any amount you pay for emergency services or out-of-network services toward your in-network deductible and out-of-pocket limit.
If you think you’ve been wrongly billed, you may contact the Ohio Department of Insurance at 800-686-1526.
Visit www.cms.gov/nosurprises/consumers or call 800-985-3059 for more information about your rights under federal law.
Billing Inquiry
Please complete the form below with any questions related to billing and a Patient Financial Services representative will contact you. In order for us to serve you better, please provide as much detail as possible when submitting the form.
"*" indicates required fields